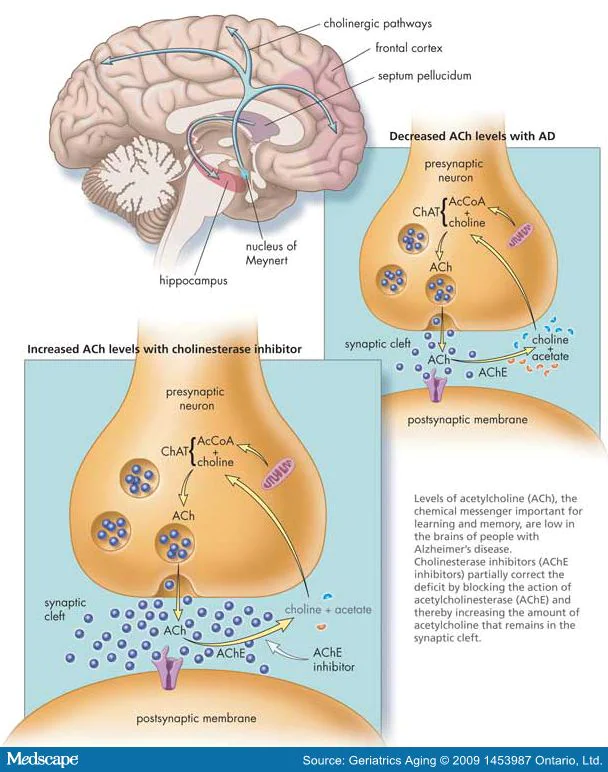
Cognition is a complex system encompassing processes such as episodic memory, working memory, executive function/inhibition, spatial learning, language/vocabulary comprehension, processing speed, and language/reading decoding. Changes in synaptic plasticity, the ability of the brain to change and adapt to new information, can be short lived from milliseconds to years. Short lived forms include facilitation, augmentation, and potentiation which enhances neurotransmitter release.
These dynamic changes represent the molecular basis for learning and memory. This synaptic plasticity can be influenced by several factors e.g., aging, diseases (obesity, diabetes, hypertension, dyslipidemia), toxins (smoking and alcohol), and exercise. Aging has been estimated to trigger performance decline with an incidence of mild cognitive impairment of 21.5–71.3 per 1000 person-years). Cortical thickness and subcortical volume are shrinking 0.5–1% annually as a morphological sign of cognitive decline with plaques and axonal degeneration. Dementia is diagnosed when the acquired cognitive impairment has become severe enough to compromise social and/or occupational functioning with increasing prevalence.
Worldwide, around 50 million people have dementia and, with one new case every three seconds, the number of people with dementia is set to triple by 2050. Thus, there is a huge need for new research in order to combat the above-mentioned metrics. The peptides below have undergone extensive research to help aid in the improvement for our neurocognitive system.
Selank
Both Selank and Semax are melanocortin’s and have pleiotropic effects involved in brain health and function. Selank by itself has traditionally been prescribed for anxiety and depression. Selank has pronounced anxiolytic activity and acts as a stable neuropsychotropic, antidepressant, and anti-stress medication.
Semax
Semax is used as a therapeutic with pathologies related to brain circulation dysfunction. As a combination, Selank/Semax has applications in improving learning processes, exploratory behavior, regeneration and development, nociceptive and in amatory processes, accelerate nerve regeneration and improve neuromuscular performance and overall neural health.